Children have been repeatedly demonstrated to have greater resistance to the most severe symptomatic responses to COVID-19. This fact contributed to the early myth that children were, in some way, immune to the effects of the disease. The largest, most comprehensive contact tracing study performed to date demonstrates this to be false; the opposite appears to be true.
A joint study performed by Princeton, University of California Berkley, Johns Hopkins University and the government of India performed contract tracing on more than 575,000 people who were exposed to roughly 85,000 verified cases of COVID-19. Their results were published in Science magazine.
Here’s their summary:
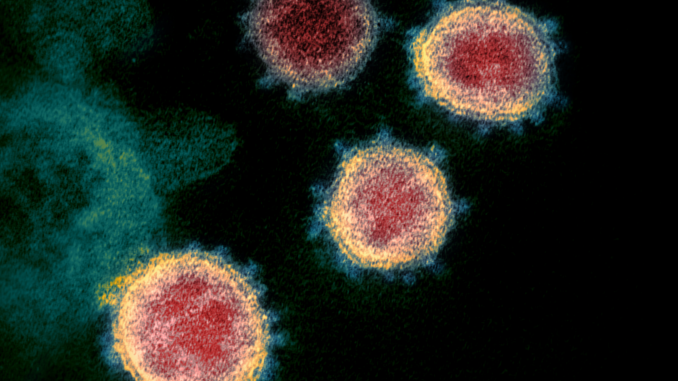
By August 2020, India had reported several million cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), with cases tending to show a younger age distribution than has been reported in higher-income countries. Laxminarayan et al. analyzed data from the Indian states of Tamil Nadu and Andhra Pradesh, which have developed rigorous contact tracing and testing systems (see the Perspective by John and Kang). Superspreading predominated, with 5% of infected individuals accounting for 80% of cases. Enhanced transmission risk was apparent among children and young adults, who accounted for one-third of cases. Deaths were concentrated in 50- to 64-year-olds. Incidence did not change in older age groups, possibly because of effective stay-at-home orders and social welfare programs or socioeconomic status. As in other settings, however, mortality rates were associated with older age, comorbidities, and being male.
Good scientists strive to be accurate and to minimize speculation. In this case, they determined conclusively that the spread was far greater among children and that, in fact, children were likely to be superspreaders of the disease. Meanwhile, the people who were more likely to die from the disease were the elderly, those with pre-existing conditions, and to a lesser degree but notably, males.
Their findings were in keeping with most other research projects, with one glaring difference: the role of children. A key difference between their research and earlier studies, though, is that they worked purely from the baseline of what people were infected and who later tested positive. Another key difference is that they were able, through the government, to test entire families instead of relying purely on volunteering individuals.
Their results suggest that perhaps economics is a factor, that for some reason the disease works differently in poorer countries than in wealthier ones. This seems contrary to the way diseases work; they no more inquire about someone’s economic status than they do a political stance. A disease spreads when the disease is given an opportunity to do so and it is present in sufficient quantity to cause infection.
In many of the studies performed in wealthier countries, they have been hindered by the use of prior assumptions. This is a sound scientific practice: by using the same assumptions that prior studies have used, new variables are minimized and better information can be gleaned from the results. But there are significant dangers when the initial assumptions are flawed, because those assumptions carry into later studies. This is why, at times, successive studies have been demonstrated to be wrong and why the verification of core data is vitally important to scientific research. Typically, everything builds on prior studies, and bad figures used at the beginning have created entire fields of mythical science, such as phrenology.
The earliest studies of COVID-19 assumed a measure of immunity for children, and minimized their inclusion. Later studies were conducted primarily in wealthier countries where parents were less inclined to allow their children to be subjected to invasive testing. Both of these factors may have produced false indicators of immunity for children, while in fact they only possess, due to their growing bodies and stronger immune systems, a heightened resistance to showing the effects.
Furthermore, “asymptomatic” is often a misnomer. It is used to describe not merely the truly asymptomatic but those with minor symptom presentation. Many who are grouped under the term display sniffles, a sore throat, coughing, and sneezing, but do not show severe reactions.
Let me break away from the analysis for just a moment to describe children. As a parent, and as a person who in their teen years was assigned to watch a decade-younger sibling, I can confirm that most children are hyperactive germ machines. They don’t cover their mouths when they cough, they pick their noses, they forget to wash their hands, and many of them don’t care about getting dirty. The youngest drool a lot. Those traits are trained out of them as they age, but especially early on they transmit diseases to each other. Every school year brings a series of colds and worse which is attributable not to the cooler weather but from the fact that they’re playing with their friends in what amount to disease pits… and this is doubly true for children at day care, where they are often sharing the same toys. They need those heightened immune systems, and I’m pleased they have them.
But children are human beings, not alien creatures. Their bodies, while growing, operate in the same way that adult bodies do. It is reasonable to believe that they who routinely catch multiple colds (another coronavirus) per year and fight them off more quickly than their parents will also catch COVID-19 and fight it off as well.
The disparity found in the massive Indian research project strongly suggests this is the case. The known flaws in many earlier studies – flaws which were intentionally repeated in most of the subsequent studies – thus suggest a grave danger in opening up the schools.
This danger is magnified when one considers the Korean contact tracing study which found that spread can happen within five minutes between unmasked people 24 feet away if they are in a ventilation path; the studies which demonstrate that standard masks only reduce viral load by about 50-70% when parties are wearing the masks (that is cumulative, though; two masked individuals transmit far less than one) and that viral load can be airborne without ventilation to a degree which causes infection at areas between 12 and 22 feet depending on factors like temperature and humidity.
Worse, the notion of fighting off COVID-19 is often misrepresented. People who have had it, including those defined as asymptomatic, are often left with severe lung damage, weakening of the heart, and capillary damage which can in turn cause problems ranging from sexual potency issues to nerve damage. These seem like terrible issues for children who may carry the effects through much of their lives.
This has not prevented governments from responding to the desires of their populace, with the blessing of scientists who have been using the studies that incorporated earlier assumptions. Greece is the latest nation recommending the opening of all secondary schools. Trump pushed hard for opening all of the schools, and Biden is promoting a similar push, although he is stressing that it must be done safely.
There is no “safe” opening of schools. More, the massive spike of cases seen in countries throughout the world may be far more attributable to the opening of schools than any other factor including weather and precautionary burnout. There are measures which can be taken to improve safety, and I applaud the desire to provide those to schools throughout the country. But the best decision would be to diminish rapid transmission through the populace by shutting down schools save for that small percentage of students who, for various reasons, cannot learn at home, leaving the classes limited to three or less students per teacher for the duration of the COVID-19 pandemic. For economic reasons that is not going to happen, and we are going to continue to deal with outbreaks.
